Gary S. Wasserman, DO
- Chief, Section of Medical Toxicology
- Professor of Pediatrics
- University of Missouri?ansas City
- Children? Mercy Hospitals & Clinics
- Kansas City, Missouri
Tulasi dosages: 60 caps
Tulasi packs: 1 bottles, 2 bottles, 3 bottles, 6 bottles

Buy tulasi with visa
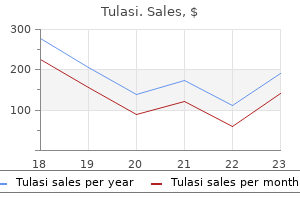
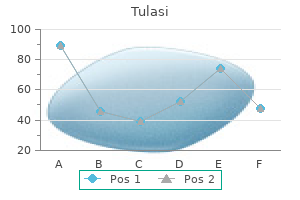
The ability to use the coronary sinus catheter to assess left ventricular preexcitation should not be neglected symptoms anemia tulasi 60 caps with mastercard. The limitations imposed by anatomic variations apply for the ventricular insertion site as well medications ending in ine purchase 60 caps tulasi overnight delivery, but are less significant treatment 197 107 blood pressure purchase generic tulasi from india. In the presence of a left-sided bypass tract, the base of the heart is activated early, simultaneously with the delta wave (Fig. Early activation usually can be distinguished in one bipolar electrogram with an accuracy of 1 cm if 5-mm interelectrode distances are used. Obviously, the most precise method of determining the site of ventricular preexcitation is via a left ventricular mapping catheter. The ventricular insertion site usually has a close relationship with the atrial insertion site, as shown by comparing the site of antegrade preexcitation with retrograde atrial activation mapping (Fig. Changes in local V-A interval due to changes in the wavefront of activation suggest a slanted bypass tract. In both cases, the ventricular insertion is usually more medial than the atrial insertion. Using unipolar recordings, the earliest intrinsicoid deflection is in pole 2, defining that pole as closest to the site of ventricular insertion of the bypass tract. Thus the site of the ventricular insertion of the bypass tract matches the atrial insertion site. Thus, the greater the proximity to the atrial insertion site of the bypass tract during atrial pacing, the greater the degree of preexcitation and the shorter the 32 88 P-to-delta-wave interval will be. For example, if activation of the atrial insertion of the bypass tract begins 80 msec after the high-right atrial depolarization, pacing the atrium at or near the site of the bypass tract will shorten that interval by approximately 80 msec. This will decrease the P-to-delta-wave time by approximately 80 msec and will produce a greater degree of ventricular preexcitation because the ventricles will begin depolarization earlier via the bypass tract. An example of how this technique can be used to localize the bypass tract is shown in Figure 10-50 in which high-right atrial pacing results in preexcitation with a P-to-delta-wave interval of 95 msec, while coronary sinus pacing produces a shortening of the P-to-delta-wave interval to 50 msec and a greater degree of preexcitation. Therefore, it is imperative that electrograms from around both the tricuspid and mitral valves be evaluated. A Halo catheter or other type of multipolar (10 to 20 poles) placed around the tricuspid annulus may be useful to guide precise mapping of right-sided pathways. A multipolar catheter recording from the os to the distal coronary sinus (near the aortic valve) can be used to guide left atrial mapping with the limitations of coronary sinus anatomy taken into consideration. Occasionally mapping of the veins off the coronary sinus is necessary to precisely localize epicardial pathways. These are not infrequently associated with structural abnormalities in the coronary sinus, for example, coronary sinus diverticulum. Both right and left atrial catheters can be moved to record along the entire circumference of the tricuspid and mitral valves to precisely ascertain the site of earliest atrial activation. This is critically important, particularly when multiple bypass tracts are suspected (see following discussion). In many patients multiple breakthrough sites are seen with simultaneous activation of the apex and base of the triangle of Koch or even the coronary 92 93 sinus , (see Chapter 8). Consequently, the left atrium will be depolarized first in the presence of a left free wall bypass tract, and the free wall of the right atrium will be depolarized first in the presence of a right free wall bypass tract (Figs. Atrial fusion due to simultaneous activation over the A-V node and bypass tract must be excluded. Furthermore, as stated earlier, the retrograde atrial activation sequence during ventricular stimulation and the comparative antegrade activation sequence during sinus rhythm occur near each other, with some differences based on whether the bypass tract is slanted. Although this site showed the shortest ventriculoatrial activation and earliest atrial activation, the catheter could not be advanced to evaluate more distal left atrial sites. This, therefore, bracketed the earliest site, proving it came from the midlateral wall. In patients with retrogradely functioning septal bypass tracts, atrial excitation may appear similar to “normal” atrial activation located in the anterior, mid, or posterior triangle of Koch, as shown in Figures 10-56 and 10-57. With posteroseptal bypass tracts, the electrogram at the os of the coronary sinus or base of the triangle of Koch will usually be slightly earlier than that recorded at the apex of the triangle of Koch. With anteroseptal, para-Hisian, or mid-septal bypass tracts, the electrogram at or near the apex or midportion of the triangle of Koch will be earlier than the base of the triangle of Koch or coronary sinus. Because both these patterns of atrial activation can be seen in an A-V nodal reentry, other methods must be used to show whether retrograde conduction is occurring over a bypass tract. Ventricular extrastimuli or pacing can help resolve the issue of what is conducting retrogradely with a “normal” retrograde atrial activation sequence.
Mauls (Mallow). Tulasi.
- What is Mallow?
- Wounds, bronchitis, stomach upset, diarrhea, irritation of the mouth and throat, and dry cough.
- Are there safety concerns?
- Dosing considerations for Mallow.
- How does Mallow work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96228
Purchase cheap tulasi
However medicine 95a pill cheap tulasi 60 caps buy online, if this relationship is not appreciated by the patient These processes differ in regard to the appearance of the and surgeon prior to blepharoplasty medications identification cheap 60caps tulasi with mastercard, the brows will descend forehead skin treatment 32 for bad breath buy cheapest tulasi, with natural aging and normal frontalis func- postoperatively, when this compensatory mechanism is no tion resulting in transverse skin rhytids, whereas the paretic longer needed. Despite the upper lid skin excision, a descend- brow is typically ptotic but without wrinkling due to ing brow can offset the rejuvenative effects of the upper decreased frontalis tone. Understanding the anatomy of the brow and gator muscles, procerus, and orbicularis oculi muscles can the etiology of the aging process is vital in achieving the lead to vertical or transverse glabellar creases, and “crow’s desired results in foreheadplasty and browlift. When mild, these conditions can be treated with Botox for improved contour and symmetry [21 ]. Moderately deep creases may be addressed with a variety of 7 Objectives alloplastic filler materials, which are not addressed in this chapter. However, deep creases and skin excess are best dealt As with much of aesthetic surgery, the aims in rejuvenative with surgically by means of browlift, with or without dener- procedures for the brow are simple, and the difficulty lies in vation of the muscles of the brow and resection of the pro- their implementation. While the use of chemical youthful appearance to the brow region, without “overplay- denervation with Botox and soft tissue augmentation with ing the hand” and conveying an overly lifted appearance. As non-autologous fillers will not be discussed in further detail Barton states in his book, while the depressed brow in unaes- here, the reader is referred to an excellent article on the topic thetic, it is natural. The goal is to elevate the elements of the brow smoothly with long-term results, and detail the limited situations in and to the correct extent. Because of the power of the brow typically needs to be lifted more than the remainder of endoscopic lift, and the well-hidden scars, coronal incisions the brow. In lifting and redraping the brow, transverse lines should be softened, and if necessary autologous or off-the- 9 Operative Technique shelf fillers can be employed to fill deeper creases. Hair fol- licle concentration and thickness should be preserved, and In the senior author’s clinical cases, the results of this ana- the hairline location should be either preserved or lifted to a tomical study of the ligamentous attachment positions are minor extent. If indicated, an upper blepharoplasty should be applied to preserve them with both open and endoscopic performed to excise excess upper eyelid skin prior to redrap- approaches. Whenever possible, the tenets detailed above rior to the hairline, dissection is performed inferiorly in the for the aesthetic brow should be the goal. Care is however, the appearance of the row and upper lids can vary taken to preserve the medial brow retaining structures. The lateral retinacular ligament is released lateral to the supraorbital nerve, avoiding any trac- tion on the nerve. Adequate exposure for resection of the 8 Approaches medial corrugators and procerus muscles is obtained by dis- secting a central tunnel between the two superomedial retain- 1962 Gonzales-Ulloa Coronal incision for forehead/browlift [3 ] ing structures. Preserving these medial retaining structures 1978 Ortiz-Monasterio Combined rhytidectomy and coronal allows the surgeon to control the position of the lateral brow browlift procedures [25 ] while helping to prevent over-elevation or lateral spreading 1994 Vasconez Endoscopic approach to browlift [26 ] of the medial brow in both endoscopic and open procedures. Gonzales-Ulloa first described the coronal approach in Once the dissection is completed, the process of brow an isolated procedure for elevation of the forehead and elevation and suspension can begin. Ortiz-Monasterio then incorporated this as an ele- ated with a small drill, which provide strong cleats through ment of his rhytidectomy technique in 1974, and many which to pass the suture. Two variations on this long coronal such as screws, posts, or anchors which could become pal- incision have become commonplace, the standard coronal pable are avoided. The suspensory sutures consist of per- incision with curvilinear deviations such that the incision manent (4-0) nylon sutures in the deep dermal plane. Three is always 6–7 cm posterior to the hairline and a modified passes of the suture are made through the deep dermis, anterior hairline incision. This modified anterior hairline aponeurotic tissues, and galea for each point of fixation. This incision is the senior author’s knot will not slip as subsequent throws are placed. Care preference in those patients with a relatively high hairline must be taken to avoid placing too much tension on these or anteriorly thinning hair. The next major advance in surgical approaches arrived with the advent of endoscopy in plastic surgery. Knize fur- 10 Closure ther refined these approaches with a limited scar technique for brow, temporal, and upper eyelid rejuvenation. These The closure of the endoscopic or limited-length incisions minimally invasive techniques are, in most cases, equally within the hair is accomplished with a skin stapler. These potent in terms of brow elevation versus the coronal incisions are everted properly, and the scars heal well with approach, with a reduced incidence of scalp paresthesias or the advantages of ease of removal and without the need to alopecia. Though fewer surgeons are relying on the coronal tie or remove sutures among the hair follicles.
Cheap tulasi
Reliability assessment of the bladder diary for urinary incontinence in older women medications related to the lymphatic system cheap 60caps tulasi with amex. Dietary caffeine intake and the risk for detrusor instability: a case-control study treatment breast cancer cheapest tulasi. Prevalence of urinary incontinence and associated risk factors in postmenopausal women treatment 1st metatarsal fracture discount 60caps tulasi mastercard. Obesity and lower urinary tract function in women: Effect of surgically induced weight loss. Gynecologic-obstetric changes after loss of massive excess weight following bariatric surgery. Changes in urinary and fecal incontinence symptoms with weight loss surgery in morbidly obese women. Long-term efficacy of nonsurgical urinary incontinence treatment in elderly women. Long-term effect of pelvic floor muscle exercise 5 years after cessation of organized training. The effect of behavioral therapy on urinary incontinence: A randomized controlled trial. Predictors of outcome in the behavioral treatment of urinary incontinence in women. Effects of pelvic floor muscle training on strength and predictors of response in the treatment of urinary incontinence. In Western countries approximately 10% of all adult women report leakage at least weekly [1]. Increasing prevalence of 20%–30% during young adult life to 30%–40% around the menopause to 30%–50% in the elderly has been reported by some authors [2,3]. Others report a prevalence of any urinary incontinence of 22% [4] to 29% [1] in older women, severe urinary incontinence in 7% [1]. Urinary incontinence is associated with nursing home admission from the community [6]. Although there is no consensus yet about what constitutes significant urinary incontinence [7], incontinence is predominantly a problem among women: 10% of them suffer from weekly incontinence, 25%–45% from occasional leakage [7]. The annual incidence of “monthly” or “any” urinary incontinence varies between 1% and 19%, for “weekly” urinary incontinence between 1. Mainly due to shame, taboo, and unawareness of treatment possibilities, only a minority of people suffering from incontinence seek professional help [9,10]. In daily general practice, patients usually go for help when the loss of urine leads to mental, physical, or social problems or discomfort for the patient or his or her social environment. Because of more and better patient information, in the Netherlands now about half of the women suffering from urinary incontinence consult a medical doctor [10]. Symptoms of the latter are urgency, frequent micturition, nocturia, and/or urgency incontinence [11]. Isolated urgency urinary incontinence is the second most prevalent cause of urinary incontinence (1%–7%) [1]. Combinations of the aforementioned symptoms of stress and urgency incontinence are considered to reflect mixed incontinence [12]. A patient suffering from stress incontinence usually has a normal voiding frequency (less or equal than eight times in 24 hours) and bladder volume and has mean micturitions between 200 and 400 cc/void, but with neither urgency nor micturition. A patient with urgency incontinence usually loses more urine (up to the complete content of the bladder) than a patient with stress incontinence. On the other hand, the patient may void less than 150 mL urine during micturition, suggesting a reduced functional capacity of the bladder. Incontinence has several treatment options such as physiotherapy, drug treatment, and surgical procedures. For the time being, little is known about the implementation of these guidelines and their use in daily practice [16]. For patients with incontinence, physiotherapy is often considered as first-line treatment due to its noninvasive character, the results in terms of symptom relief, the possibility of combining physiotherapy with other treatments, the low risk of side effects, and the moderate to low costs.
Buy tulasi 60 caps otc
During pregnancy the endopelvic fascial attachments of the bladder neck and distal sphincter are weakened possibly due to hormonal influences [2] 897 treatment plant rd cheap tulasi 60caps buy online. Progesterone reduces urethral closure pressures and produces connective changes [3 treatment of bronchitis discount tulasi 60caps with amex,4] that probably contribute to the high incidence of any antenatal incontinence symptoms you may be pregnant order tulasi 60caps line. If the endopelvic fascial attachments and sphincter function are not damaged at delivery, then the changes seen antenatally are likely to revert to the nonpregnant state with the return of urethral function and continence. However, if these structures are damaged or are inherently weak in the nonpregnant state, then recovery might not arise. Support for this hypothesis comes from studies suggesting the presence of a constitutional factor, e. This, along with further deliveries, aging, menopause, and muscle weakness, seems to increase the risk of long-term incontinence [10]. In a study of women reassessed 6 years after childbirth [13], there was a rate of new-onset incontinence of approximately 30% in women who had been continent at 3 months postpartum. However, in 27% who were incontinent at 3 months, there was spontaneous remission at 6 years. Of particular interest were those women who were incontinent prior to pregnancy; there was a markedly increased risk for leakage at 6 years. These interesting findings suggest that there are women at risk of incontinence, while in others there is spontaneous remission. Based on data from a systematic review, during the first 3 months postpartum, the pooled prevalence of any postpartum incontinence is 33%, with longitudinal studies showing small changes in prevalence in the first year after childbirth [5]. A larger 2-year study of 64,650 women aged 36–55 years showed complete remission in 13. A 2-year study of noninstitutionalized women over 60 years showed a 1- year remission rate of 12% [24]. A study followed 2025 women aged over 65 years for 6 years (baseline prevalence of urgency incontinence was 36. This study showed for urgency incontinence, the 3-year incidence and remission rates between the third and sixth years were 28. For stress incontinence, the 3-year incidence and remission rates between years 3 and 6 were 28. A longitudinal Swedish population-based study of over 100 women from 1991 to 2007 showed incidence and remission rates of 21% and 34%, respectively [14]. The reported incidence for cystocele is around 9 per 100 woman-years, 6 per 100 woman-years for rectocele, and 1. A 4-year observational study [27] in postmenopausal women showed an overall 1- and 3-year prolapse incidence of 26% and 40%, respectively. This study [27] also showed a 1- and 3-year resolution risk of 21% and 19%, respectively. The study also showed that over 3 years, the maximum vaginal descent increased by at least 2 cm in 11% of the women and decreased by at least 2 cm in 2. In older age groups (>70 years), many are symptomatic and approximately 11% will undergo surgery, but there are few data on the numbers treated conservatively, e. The majority (78%) demonstrated no change in the leading edge of the prolapse between the first and the last visit, following which 63% still continued observation [32]. Prevention can be classified as primary (interventions in asymptomatic individuals to reduce known risk factors for the development of a disease) or secondary (to detect symptoms at an early stage and to intervene to stop further development or to improve the prognosis of the condition). To stop recurrence of an illness or preventing it becoming chronic is tertiary prevention. There are known predisposing factors such as age, obesity, family history, parity/vaginal childbirth, and surgery. Identification of individuals at risk might help with implementing preventative measures. Although the prevalence of incontinence is increased in the elderly, the two do not necessarily have a cause-and-effect relationship; other pathological processes associated with aging might be responsible. Likewise, management of other risk factors such as chronic cough, smoking, and adjusting medication that has an adverse effect on the bladder could help incontinence (e.
Buy tulasi toronto
Each in- In 1930 thereafter symptoms 9 dpo generic tulasi 60 caps, the selective theories re- dividual antigenic determinant of the vari- surfaced treatment 6th feb discount tulasi 60 caps amex. In selective function of antigen in his natural se- some cases medicine qid 60 caps tulasi order with amex, an idiotope may be the actual lection theory. According to Jerne, million of antigen-binding site and in some cases, an globulin (antibody) molecules were formed idiotope may comprise variable region se- in embryonic life, which covered the full quences outside the Abs. These anti- contain multiple idiotopes, the sum of the bodies were natural antibodies. When anti- individual idiotopes is called idiotype of gen was introduced, it combined selectively the antibody. In this theory, selection was so on, forming a idiotype network, which postulated in the level of antibody molecule, is postulated to regulate the antibody syn- but not in the cell. If the individual lymphocyte expresses membrane theory of one gene-one antibody molecule receptor that is specific for a distinct antigen. The ferent segments of the light (L) and H chains, phenomenon of split genes explains this. The it is possible to have antibodies with far more genetic information for the synthesis of immu- than 108 types of specificities. The split gene noglobulin molecule is not present in a con- shuffling takes place during cell development tinuous array of codons. For example, the kappa L chain genes in genetics and has important implications are composed of three separate segments V, in biology, beyond immunology. There are about a hundred different covery, Susumu Tonegawa was awarded the types of variable (V) domine sequences and Nobel prize in medicine in 1987. What happens when B cell responds to indromic arrangement (sequences that can be a foreign antigen? How do functions of attached by either end), it is possible to gen- plasma cells and memory cells differ? How do the primary and secondary re- The lambda chain has additional C sequenc- sponses to the same antigen differ? The heavy (H) chain gene has also a diver- is the significance of those differences? Current Protocols in Immunology, New macrophages and dendritic cells play York: Wiley; 1997. Immunological Tolerance 10 Immunological tolerance is a state of unre- They also postulated that tolerance sponsiveness to a particular antigen to which could be induced, if some foreign antigens a person has been exposed earlier. The im- are administered during embryonic life and portant aspect of tolerance is the self-toler- also in neonates. Medawar and his col- ance, which prevents the body to mount im- leagues in 1953, further supported the ex- mune response against self-antigens. Since, periment inducing immunological tolerance the immune cells (lymphocytes) possess vast to skin allografts (grafts that are genetically diversities of antigen receptors, it is possible not similar) in mice by neonatal injection of that some receptors may be self-reactive. Hence, the key factor de- The first evidence of self-tolerance was termining the tolerance is not the develop- introduced by Traub in 1938, who in- mental stage, but the state of maturity of the oculated mice, in utero, with lymphocytic immune cells (lymphocytes) at the time of choriomeningitis virus producing infection the encounter of the antigen. These neonates, the immune cells are still to ma- inoculated mice, unlike normal mice did ture and therefore, the individual remains not produce neutralizing antibodies against unresponsive at this stage. Each of the twins had erythrocytes of its own and In the thymus, proliferation and massive death others blood group, as there is exchange of thymocytes takes place simultaneously. There- Self-reactive cells, some times ignore the fore, there must be some negative selections, presence of self-antigen. The circumstances which operate simultaneously to silence the in which the presence of antigen is ignored self-reactive lymphocytes. It has long been established that when an immature B cell comes in contact with the self-antigen, there is cross-linking of mem- brane immunoglobulin M (mIgM) leading to the death of the cells in the bone marrow (negative selection). Later work by other researchers using transgenic system described by Nemazee and Biirki, showed the negative selection of Fig. Changes are able to resume rearranging their light that favor the development of Th1 like cell- chain genes. As a result, these cells will begin Tolerance to self-epitopes can also be to express an ‘edited’ mIgM with a different induced by regulatory cells. In most cases, light chain and specificity that is not self-re- the regulatory cells are T cells. They and leave the bone marrow as mature B cells play important role in preventing inflamma- bearing the edited non-self-reactive mIgM.
Cheap tulasi 60 caps with visa
Other assessments: Synchronous ultrasound screening of the bladder and/or urethra and measurement of the bladder and Pabd during filling and voiding cystometry medicine search purchase tulasi online now. Anal ultrasound (endosonography) [42]: This is the gold standard investigation in the assessment of anal sphincter integrity medications not to take when pregnant generic tulasi 60caps amex. There is a high incidence of defecatory symptoms in women with anal sphincter defects treatment ind effective tulasi 60 caps. Intravenous urography [43]: This provides an anatomical outline of the urinary tract including a nephrogram prior to passage of the contrast to the calyces, renal pelvis, ureter, and bladder. Micturating cystogram [44]: The principal use is the detection of vesicoureteric reflux, some fistulae, and diverticula. Defecography [42]: This demonstrates normal anatomy of the anorectum as well as disorders of rectal evacuation. Measurement of the anorectal angle is allowed with evidence of the presence, size, or emptying of any rectocele. Enteroceles, rectal intussusception, and mucosal prolapse might be diagnosed as well as a spastic pelvic floor (anismus). Colporectocystourethrography (colpocystodefecography) [43]: This involves the instillation of radiopaque media into the bladder, vagina, and rectum simultaneously for pelvic floor evaluation with images obtained during rest and straining. It is noninvasive, has excellent soft tissue contrast resolution without exposure to ionizing radiation, and allows the study of function of pelvic floor structures under different dynamic conditions such as increased Pabd during Valsalva [45,46]. Currently, the clinical value of these examinations is still under investigation with its impact on therapeutic decisions not yet fully evaluated. Bladder neck and cervical descent/mobility – Position of bladder neck and cervix at rest and on Valsalva. Bladder neck or cervical descent >2 cm below this line with straining indicates weakness of the pelvic floor. If alternative landmarks are used in scientific papers, they should be clearly described. Pelvic floor measurements/levator defects: Assessment of the configuration of pelvic floor muscles, in particular, the levator ani. A: Urodynamic Stress Incontinence Definition: As noted in Section 3E(2d), this diagnosis by symptom, sign, and urodynamic investigations involves the finding of involuntary leakage during filling cystometry, associated with increased intra- 1802 † abdominal pressure, in the absence of a detrusor contraction. Bladder Oversensitivity Definition: Bladder oversensitivity, a diagnosis made by symptoms and urodynamic investigations, is more likely to occur in women with symptoms of frequency and nocturia and a voiding diary showing a clearly reduced average voided volume. Also referred to as “increased bladder sensation” [3], bladder oversensitivity replaces the now obsolete term of “sensory urgency” [50,51]. As noted in Section 3D(3f), it can be defined as an increased perceived bladder sensation during bladder filling 1C(1) with specific cystometric findings of (1) an early first desire to void 3D(3b); (2) an early strong desire to void, which occurs at low bladder volume 3D(3d); (3) a low maximum cystometric bladder capacity 3D(4b); and (4) no abnormal increases in Pdet [50,51]. Specific bladder volumes at which these findings § occur will vary in different populations. Definition: Voiding dysfunction, a diagnosis by symptoms and urodynamic investigations, is defined as abnormally slow and/or incomplete micturition [53]. Abnormal slow urine flow rates and abnormally high postvoid residuals, the basis of this diagnosis, are outlined in Sections 3A(10) and 3B(3). This diagnosis should be based on a repeated measurement to confirm * abnormality. Further evaluation—pressure–flow studies (voiding cystometry): Pressure–flow studies are indicated to evaluate the cause of any voiding dysfunction. Some possible causes have been already defined: 3F(3b) detrusor underactivity, 3F(3c) acontractile detrusor, and 3G(2) bladder outflow obstruction. Acute retention of urine [3]: This is defined as a generally (but not always) painful, palpable, or percussible bladder, when the patient is unable to pass any urine when the bladder is full. The standardisation of terminology of lower urinary tract function: Report from the standardisation subcommittee of the International Continence Society. The standardization of terminology for researchers in female pelvic floor disorders. Definition and classification of urinary incontinence: Recommendations of the Urodynamic Society. Report of the international consensus development conference on female sexual dysfunction: Definitions and classifications. Sexual function in women with/without urinary incontinence and or pelvic organ prolapse.
Syndromes
- A sharp or broken tooth or poorly fitting dentures
- Gastric lavage
- Age 9-13 years: 4* mg/day
- Dementia
- Nausea
- Crying, feeling sad or hopeless, and possibly withdrawing from other people
- Begins at an early age
- Blood glucose level
Cheap tulasi online amex
This usually involves a timed medicine cabinet shelves tulasi 60caps order visa, measured void medicine 219 buy 60 caps tulasi fast delivery, followed by 1252 urethral catheterization or bladder ultrasound to measure postvoid residual urine volume treatment 3rd degree burns tulasi 60caps. If surgery to repair the prolapse is planned, it is important to check urethral function after the prolapse is repositioned. Women with severe prolapse may be paradoxically continent because of urethral kinking; when the prolapse is reduced, urethral dysfunction may be unmasked with occurrence of incontinence (occult stress incontinence) [20]. A pessary, vaginal retractor, or vaginal packing can be used to reduce the prolapse before office bladder filling or electronic urodynamic testing. If urinary leaking occurs with coughing or Valsalva maneuvers after reduction of the prolapse, the urethral sphincter is probably incompetent, even if the patient is normally continent. In this situation, the surgeon should consider adding an anti-incontinence procedure in conjunction with anterior vaginal prolapse repair [21]. If stress incontinence is not present even after reduction of the prolapse, an anti-incontinence procedure probably still decreases the rate of postoperative urinary incontinence but results in more complications, voiding dysfunction, and higher cost [21,22]. A validated, individualized computer prediction model for de novo stress incontinence after prolapse surgery is available [23]. Modifications of the technique depend on how lateral the dissection is carried, where the plicating sutures are placed, whether apical support is added, and whether additional layers (natural or synthetic grafts) are placed in the anterior vagina for extra support. The operative procedure begins with the patient supine, with the legs elevated and abducted and the buttocks placed just past the edge of the operating table. Antibiotics should be given within 60 minutes of incision to achieve minimal inhibitory concentrations in the skin and tissues by the time the incision is made. This typically means a first-generation cephalosporin (cefazolin) or combination regimens (500 mg metronidazole and 400 mg ciprofloxacin) if the patient has an allergy to penicillin [24]. In general, all patients undergoing vaginal prolapse surgery are at moderate risk for thromboembolic events and require a prevention strategy [25]. Low-dose unfractionated heparin (5000 units every 12 hours), low- molecular-weight heparins (e. Either form of heparin should be started 2 hours before surgery and the compression stockings placed on the patient in the operating room before incision. The abdomen, vagina, and perineum are sterilely prepped and draped, and a 16 Fr Foley catheter with a 10 mL balloon is inserted for easy identification of the bladder neck. If a vaginal hysterectomy has been performed, the incised apex of the anterior vaginal wall is grasped transversely with two Allis clamps and elevated. Otherwise, a transverse or diamond-shaped incision is made in the vaginal epithelium near the apex. A third Allis clamp is placed about 2 cm below the posterior margin of the urethral meatus and pulled up. If a midurethral sling is to be done, then the incision is only made to the bladder neck; a separate incision is made for the sling. Additional Allis clamps may be placed in the midline between the urethra and apex. Alternatively, the points of a pair of curved Mayo scissors are inserted between the vaginal epithelium and the vaginal muscularis, or between the layers of the vaginal muscularis, and gently forced upward while being kept half opened/half closed (Figure 82. Countertraction during this maneuver is important to minimize the likelihood of perforation of the bladder. The vagina is incised in the midline, and the incision is continued to the level of the midurethra (or bladder neck if a sling is being done). As the vagina is incised, the edges are grasped with Allis or T-clamps and drawn laterally for further mobilization. Dissection of the vaginal flaps is then accomplished by turning the clamps back across the forefinger and incising the vaginal muscularis with a scalpel or Metzenbaum scissors, as shown in Figure 82. An assistant maintains 1253 constant traction medially on the remaining vaginal muscularis and underlying vesicovaginal adventitia. This procedure is performed bilaterally until the entire extent of the anterior vaginal prolapse has been dissected; in general, the dissection should be carried further laterally with more advanced prolapse. The spaces lateral to the urethrovesical junction are sharply dissected toward the ischiopubic rami. It is also important to use sharp dissection to mobilize the bladder base from the vaginal apex as shown in Figure 82. If the patient does not suffer from stress urinary incontinence, plicating sutures at the urethrovesical junction could be placed to augment posterior urethral support and to help ensure that stress incontinence, if not present at the time of operation, does not develop postoperatively.
Tulasi 60 caps order without prescription
The operation never caught on—presumably because of its perceived difficulty and the concurrent emergence of simple and effective midurethral slings medicine lookup tulasi 60 caps order mastercard. It is never quite clear in retrospect who made the first contribution since one relies entirely on what others have written on the subject treatment head lice tulasi 60 caps order free shipping. Modifications of this technique were practiced in some centers until fairly recently [86] treatment 2nd degree burn purchase tulasi line. The gracilis muscle was also used as early as 1907 [87], and these tendon and muscle, innervated or otherwise, have repeatedly been used over the years to wrap both the urethra and the anorectum, but suffer from the extent of dissection and mobilization required, the bulk of tissue requiring accommodation in the new site, and overall poor results. A placard shaped incision is made with its base at the bladder neck and narrow edge distally to expose the paraurethral fascia. Four separate helical sutures are used to gather up the endopelvic fascia, pubocervical fascia, and the subdermal layer of the vaginal wall. The mechanism of action of sling procedures has always been a subject of debate and uncertainty. Early wrappings with denervated muscle of one kind or another may have simply provided additional passive resistance, but subsequent designs in which slings were passed around the suburethra, at whatever level, and fixed above to an immovable structure, may have offered either passive occlusion during straining or possibly a dynamic component as well. The concept of a dynamic effect is that abdominal straining involves rectus muscle contraction, which will pull upward on the attached sling, thereby elevating the bladder neck for the duration of the contraction. All slings therefore have the potential to obstruct the urethra or simply to provide passive occlusion 1097 during moments of stress. It is a feature of all biological materials, whatever their provenance, to have the potential to shrink/contract by up to 30% of their initial length. Shrinkage of this degree will obviously further elevate the bladder neck or urethra and risk causing voiding difficulty. The tendency may be more marked with some tissues than others, but this has not really been established. Every sling material should have more or less the same effect to begin with, but the specific material used evidently matters in terms of its capacity for shrinkage, infection, erosion, and subsequent stretching or failure, while the amount of tension applied to the sling and its positioning will possibly adversely affect filling and voiding function. Whether slings are inserted from top-down or bottom-up appears to make little difference though there is evidence that the more extensive the vaginal dissection required, the more likely it is that innervation will be disturbed [87]. Thus, strips of fascia were created at least 10 cm in length on each side (Figure 70. A midline suburethral vaginal incision was then made to expose the pubocervical fascia and dissection continued cranially toward the retropubic space. A midline colporrhaphy was first performed to provide bulking of tissue under the urethra, and the ends of the rectus strips were then passed downward through the retropubic space on each side to emerge into the vaginal incision on either side of the urethra. Here, they were then sewn together under the urethra to provide elevation and support of the urethra. Of course, in the finest surgical tradition, the procedure has been much modified, a neat idea being that used by Warrell in which dissection of the medial component of the rectus strip was angled downward to create additional length, thereby also reducing the need for lateral dissection (Figure 70. Lateral dissection in the original procedure was complicated by the thinness of external oblique fascia beyond the lateral border of the rectus sheath and the risk of lateral angle pain postoperatively. Leaving the sling attached at one end obviated any need for fixation except under the urethra, but this created difficulties in establishing the correct amount of tension; in addition, there were times when sometimes the sling would not reach the vagina. During his dissection of the vaginal end, he deliberately opened the bladder in order to prevent damage to it, a surprising suggestion coming several years after Stamey popularized peroperative endoscopy, in part, for the same reason. Blaivas also reported the use of a free graft [89], and, between them, these two surgeons radically influenced surgical practice throughout the United States over the next 20 years. The reasons for this were the growing awareness of poor long-term outcomes from needle suspensions and that a fascial sling would be effective in women with either hypermobility or intrinsic sphincter weakness or both. It became known that slings with less tension remained effective but with diminished likelihood of postoperative voiding dysfunction, which remained a problem for retropubic suspensions. Full-Length Autologous Rectus Fascial Sling: Technique The procedure described is that used throughout the 1990s; inevitably, modifications took place with the adoption of ideas from others and the growing realization that tension should be minimal and the midurethral rather than bladder neck support was the objective (Figure 70. A degree of Trendelenburg 1099 tilt in the operating table provides a good view of the anterior vaginal wall and helps to autoretract any abdominal fat apron. Particularly, fatty labia may be temporarily gently sutured laterally to provide a good vaginal view. The bladder is catheterized, following which the anterior vaginal wall infiltrated with 1:200,000 epinephrine in saline solution. This may then be left for a few minutes while the abdominal dissection takes place (Table 70. Before dividing the fascial strip laterally, a transfixion suture of 2-0 nonabsorbable material is used to bind the tissues together.
Buy 60caps tulasi mastercard
Enterocele is not a contraindication to stapled transanal surgery for outlet obstruction: An analysis of 170 patients medicine keflex cheap 60 caps tulasi amex. Minimally invasive treatment of urinary stress incontinence and laparoscopically directed repair of pelvic floor defects treatment dvt cheap tulasi 60 caps on-line. Transvaginal repair of enterocele and vaginal vault prolapse using autologous fascia lata graft symptoms checklist 60caps tulasi buy fast delivery. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Site-specific fascial defects in the diagnosis and surgical management of enterocele. High uterosacral vaginal vault suspension with fascial reconstruction for vaginal repair of enterocele and vaginal vault prolapse. Posterior colporrhaphy is superior to the transanal repair for treatment of posterior vaginal wall prolapse. Transanal or vaginal approach to rectocele repair: A prospective, randomized pilot study. Sacrospinous ligament fixation for massive genital prolapse in women aged over 80 years. Prospective randomized trial of polyglactin 910 mesh to prevent recurrence of cystoceles and rectoceles. Abdominal sacral colpopexy in 163 women with posthysterectomy vaginal vault prolapse and enterocele. Surgical support and suspension of genital prolapse, including preservation of the uterus, using the Gore-Tex soft tissue patch (a preliminary report). Abdominal sacral colpopexy or vaginal sacrospinous colpopexy for vaginal vault prolapse. Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: A prospective randomized study with long-term outcome evaluation. Uterine preservation or hysterectomy at sacrospinous colpopexy for uterovaginal prolapse? Long-term outcome of vaginal sacrospinous colpopexy for marked uterovaginal and vault prolapse. Sacrocolpopexy for vault prolapse and rectocele: Do concomitant Burch colposuspension and perineal mesh detachment affect the outcome? Rectoanal intussusception: Presentation of the disorder and late results of resection rectopexy. Since the early nineteenth century, surgeons have performed posterior colporrhaphy to manage tears of the perineum. The supports of the genital organs were largely a mystery, and there was little distinction between prolapse of the rectum, bladder, and uterus. As anatomic concepts developed, surgeons ascertained that the main support of the uterus was the vagina, which in turn is supported by the insertion of the levator ani muscles into the perineum. This concept was the basis for the incorporation of plication of the levator ani muscles into posterior colpoperineorrhaphy, with the surgical goals of restoring the anatomic support of the vagina and rectum without compromising functionality. Until recently, very little attention has been given to the functional derangements that are commonly associated with rectoceles. In 2010, an estimated 166,000 women underwent surgery for pelvic organ prolapse with a rectocele procedure occurring in approximately half of the cases [1]. A rectocele is an outpocketing of the anterior rectal and the posterior vaginal wall into the lumen of the vagina and is fundamentally a defect of the rectovaginal septum, not of the rectum. Some rectoceles may be asymptomatic, whereas others may cause such symptoms as incomplete bowel emptying, sensation of a vaginal mass, pain, and pressure. The size of the defect does not necessarily correlate with the amount of functional derangement or severity of bowel symptomatology [4,5]. This chapter reviews the anatomy, pathophysiology, diagnosis, and management of rectoceles. This layer of connective tissue is fused to the undersurface of the posterior vaginal wall. Histologically, the rectovaginal septum shows that the distal portion contains dense connective tissue; the midportion contains fibrous tissue, fat, and neurovascular tissue; and the proximal portion is mostly fat cells [7]. Posterior to the rectovaginal septum lies the rectovaginal space, which provides a plane for dissection.
Best purchase tulasi
The most prevalent type of incontinence was stress incontinence (57%) followed by urge (23%) and mixed incontinence (20%) in treatment 1 cheap 60 caps tulasi with visa. The type of toilet used and the place of residence were not found to be related to the occurrence of the condition (Table 6 medicine xarelto order on line tulasi. Age Increasing age was found to be significantly related to the occurrence of incontinence medications starting with p quality 60 caps tulasi. There was a significant correlation between the increasing prevalence of incontinence and higher parity. Number of Vaginal Deliveries Taking into account vaginal deliveries (including forceps delivery), there was a significant relationship of increasing prevalence of incontinence with a higher number of deliveries. Occupation The prevalence of incontinence was highest among those doing manual labor (see Table 6. This was found to be statistically significant, with a woman who has done manual labor at 1. Family History The family history of incontinence was significantly related to the occurrence of the condition. Family Income A higher prevalence of incontinence was found among those from the lower-income group, which was found to be statistically significant. Thus, it is worthwhile investing time and effort to study the problem, its causes, and its management (Figures 6. Types of Incontinence: Comparison with World Figures The proportion of females with stress incontinence in relation to the other types appears to be relatively low compared to previous studies citing numbers as high as 50%. This may be due to the fact that the population surveyed is relatively young while stress incontinence is more associated with advancing age. Thus, closer attention to the problem of mixed incontinence may be necessary, being the more prevalent type among Asian females [55–57]. It must be recognized, however, that the classification of incontinence used in many of these surveys is based mainly on symptoms alone and not on any objective parameter. This is a limitation inherent in the study design, as previous studies have noted that symptoms alone do not accurately classify incontinence. Therefore, further studies must be done to verify the discrepancy in the distribution of the different types of incontinence among Asian females compared to their Western counterparts. The factors found to be related to the occurrence of incontinence were not unexpected. Older age, higher parity, higher number of vaginal deliveries, the increased physical strain associated with manual labor, and the use of a sitting toilet have all been cited and accepted as contributing to the weakness of the pelvic floor leading to incontinence [58]. Aging has been associated with the loss of striated muscle in the area of the urethra leading to impaired continence. The change in the hormonal milieu brought about by aging also affects the ability of the urethral submucosal layer to provide the watertight closure of the female urethra. Childbearing, childbirth [59], and physical straining have been found to cause hypermobility, innervation injuries [60], and connective tissue changes [61] to the pelvic floor leading to loss of support. It is difficult to explain the reason behind the relationship between family income and the occurrence of incontinence. This factor may be related to parity, with those belonging in the lower-income bracket having a higher parity. While this observation is an interesting finding, this high figure may be due to the fact that this survey is institution-based and the population surveyed may be those who are motivated to seek a medical consultation for any disease 103 condition. Therefore, a community-based survey must be undertaken in order to verify this finding. It is interesting to note that almost one-fifth of those seeking help do so by seeing a traditional medical practitioner. This underscores with high regard that the Asian patient still gives to traditional medical science despite decades of Western medicine with its advances. This is important in the creation of efficient and effective programs that aim to encourage the affected population to find the solution to their problem. A more objective assessment and a clinical study of the disease must be undertaken to completely understand its pathophysiology. In addition, a deeper and more exhaustive analysis of the attitude of the population toward the disease and the reasons for seeking consult is warranted.
Avogadro, 64 years: Ablation of left-sided bypass tracts is most commonly performed from a ventricular approach in which the electrode through which energy is delivered is placed at the mitral annulus under the mitral valve.
Malir, 23 years: These wounds were produced by bullets exiting the body where the skin’s sur- face is supported (e.
Sancho, 33 years: These countries accounted for more than two-thirds of the total number of publications in the 54 African countries.
Topork, 51 years: The difference between the uterosacral vault suspension and the McCall culdoplasty rests on the obliteration of the cul-de-sac.
Phil, 43 years: Although the term bundle branch block is standard nomenclature, the pathophysiology of this electrocardiographic pattern should be thought of in terms of relative conduction delay (of varying degree and including failure of conduction) producing asynchronous ventricular activation without necessarily implying complete transmission failure.
Ivan, 24 years: Conduction to the ventricle over the A-V conducting system then will depend on antegrade conduction time over the A-V conducting system and ventricular refractoriness.
Armon, 65 years: The influence of bladder volume on the position and mobility of the urethrovesical junction.
Shakyor, 36 years: Although electrical stimulation appears to be better than placebo, its effect in stress incontinence has not been sufficiently demonstrated due to inconsistency in study protocols [43,72].
Jack, 58 years: Gram staining can be a useful alternative; the presence of bacteria can be confirmed and indicative of the causative microorganism.
Gonzales, 30 years: Where the body attempts to localize the disease, pain- given a single large dose of this drug to destroy the majority less nodules appear.
Kurt, 62 years: This directive translates to aircraft with a capacity of approxi- mately 30 passengers.
Hernando, 60 years: Late fractionated potentials and continuous electrical activity caused by electrode motion.
Julio, 39 years: Sizers are used intraoperatively to identify the largest implant the body will accommodate without creating excessive mus- cle tension at closure.
8 of 10 - Review by H. Raid
Votes: 53 votes
Total customer reviews: 53
References
- Shimizu N, Inada K, Nakanishi H, et al. Helicobacter pylori infection enhances glandular stomach carcinogenesis in Mongolian gerbils treated with chemical carcinogens. Carcinogenesis 1999; 20:669.
- Salkic S, Batic-Mujanovic O, Ljuca F, et al. Clinical presentation of hypertensive crises in emergency medical services. Mater Sociomed. 2014;26(1):12-16.
- Ogden, C.W., Reddy, P., Johnson, H., Ramsay, J.W., Carter, S.S. Sham versus transurethral microwave thermotherapy in patients with symptoms of benign prostatic bladder outflow obstruction. Lancet 1993;341:14-17.
- Hartwell SW, Hall MD. Mandibular condylectomy with silastic rubber replacement. Plast Reconst Surg 1974;53:440-444.
- Pascal RR, Hertzler G, Hunter S, et al. Pseudoinvasion with high-grade dysplasia in a colonic adenoma. Distinction from adenocarcinoma. Am J Surg Pathol. 1990;14(7):694-697.